COVID-19 and the Right to Health in Lebanon: Charity Logic the Sidelining of State

In over 80% of cases, COVID-19 does not pose a risk to the patient’s life or require hospitalization. Rather, its danger lies in its rapid spread, which inundates unprepared health systems with a large number of cases demanding medical treatment. Hence, the technical development of the medical system is not enough to avert its risks. Despite their advancement in science and medicine, many systems today appear unable to protect the lives of people due to the public policies adopted, particularly those concerning the right to health.[1] The current situation in the United States of America is a prime example.
Hence, it is now evident that the challenges in confronting COVID-19 are not merely scientific (despite the importance of the invention of vaccines that are now being rolled out in many countries). Rather, they are primarily public policy challenges. This virus has unequivocally exposed the health policies adopted around the world and the forms of health systems developed over past decades. It has raised two pivotal questions: How quantitatively and qualitatively ready are hospital systems to accommodate cases requiring medical treatment? And to what extent can people access testing and medical treatment?
In Lebanon, the virus has confronted society with the same two questions. However, the Lebanese situation is unique in the sense that for at least 30 years,[2] the political system has been anchored in two ideas. The first is fear-mongering. The second is depriving citizens of their rights and turning them into “subjects” whom the zuama [elite political leaders] can easily rally into sects using promises of protection (including security and military protection, and economic and social protection) through clientelism and patronage.
Social security is a socioeconomic necessity and a human right enshrined in international laws and charters,[3] and it is closely linked to the right to health. Nevertheless, more than half of Lebanese people (53%) have no form of regular health coverage and are therefore deprived of access to essential health services.
These people are compelled to resort to the Ministry of Public Health to benefit from its “assistance”.[4] While the decree governing the ministry tasks it primarily with “maintaining and promoting public health by providing disease prevention, … supervising private health institutions in accordance with the laws pertaining to them, [and] preparing proposals to legislate and amend laws and regulations concerning all fields of public health”, it also tasks it with treating the sick, albeit only the “needy” among them.[5] Successive governments have erected an enormous structure on the tangential power of the ministry to “treat the needy sick” such that it provides assistance in health coverage to more than two million Lebanese. Consequently, the various political forces involved in forming governments fight over this ministry and its power to control the provision of health coverage to half the population.
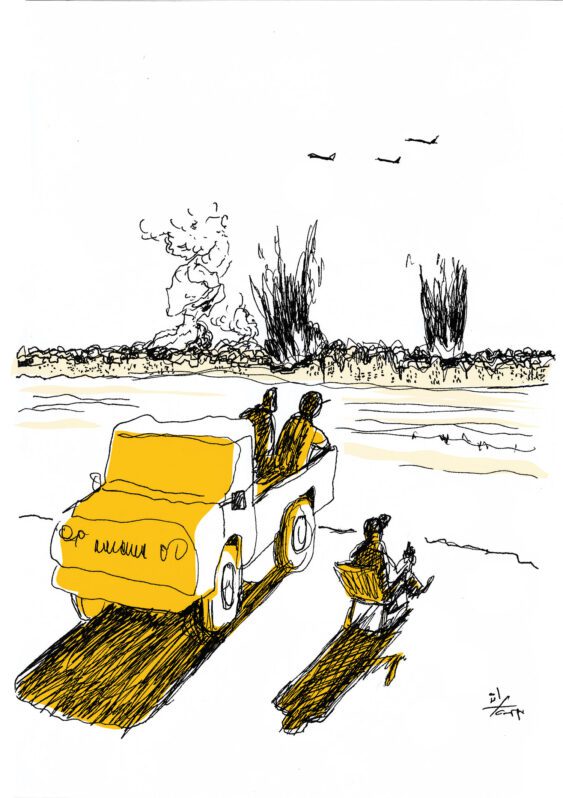
The pandemic came on the heels of an enormous popular uprising, which began on 17 October 2019. Uprising demands included accountability and political change in light of the extent of the regime’s bankruptcy and the extensive losses it has inflicted on society (causing the worst financial, monetary, and socioeconomic crisis in Lebanese history) came to light. And so emerged the risk that the regime, reeling since October 17, would attempt to catch its breath and exploit the situation created by the pandemic to reproduce itself.
Given all the above, this article searches for answers to the two aforementioned questions and links them to the current political system. First, it will examine how the traditional authorities and systems have handled the pandemic. Then it will address what we must push for today.
An “Authority” Floundering Amid Limited Possibilities
When the pandemic arrived in Lebanon in late February and the minister of public health announced the first case, the situation of the health sector and access to health coverage was as described above. The “authority” floundered, and still is, amid the limited possibilities available, and the zuama and political parties seized the opportunity to reclaim their positions of power and grasp over society by supplanting the state.
The importance of administering PCR tests to help effectively limit the virus’ spread quickly became evident. Testing, as well as inpatient treatment, was initially restricted to the Rafik Hariri University Hospital (Beriut’s main public hospital) and was free of charge. However, very strict conditions were adopted for testing, including that the person have arrived from an infected country, have been in contact with a person confirmed to be infected, or be manifesting obvious symptoms. As pressure on the public hospital increased, testing was expanded to several private hospitals, particularly university hospitals,[6] albeit for a fee (capped by the Ministry of Public Health at LL150,000, i.e. USD100 per the central bank’s exchange rate). The public hospitals also backtracked on free testing, and the price in the public sector was set at LL100,000. As for people unable to afford the test, Ministry of Public Health sources confirmed that a citizen hotline was established for testing at the ministry’s expense provided that the person concerned was symptomatic.
The retreat from free testing and its restriction in the aforementioned manner deters many people (especially asymptomatic carriers) from accessing the test and therefore negatively affects public safety. Moreover, it violates Contagious Diseases Law no. 0/1957. The law’s Article 9 stipulates that if an epidemic threatens the republic or spreads within it and local means of prevention are insufficient, the government shall bear “the expenses of implementation [of the measures adopted], whether for people, equipment, or supplies, and the major municipalities shall bear one quarter of these expenses”.
After speaking to reliable medical sources, sources within the Ministry of Public Health, and insurance sector personnel, I have several observations.
Regarding access to testing:
- In the initial stage, when testing was restricted to the Rafik Hariri University Hospital, many people hesitated to undergo testing because of distrust caused by public policies that have neglected public hospitals for decades (despite the consensus that the Rafik Hariri University Hospital performs good work today). The restriction of testing to this hospital also reduced access to many people located far from the capital. While increasing the number of hospitals authorized to administer the test, including public hospitals in the regions, could facilitate more access, the chronic neglect and shortage in equipment and staff due to the same policies prevented them from performing their role and prompted some to seek assistance from private hospitals.[7] Furthermore, infected people only underwent testing when they manifested symptoms that compelled them to go to emergency departments. In such cases, the cost of examination in the emergency department was added to the test’s cost, bringing the total bill to the equivalent of LL300,000.
- However, as the virus spread and case numbers rose (especially during the second wave, i.e. after the virus began spreading once again after declining in early July), testing increased and expanded to the private sector, which saw it as an opportunity to make huge profits. The number of tests administered each day reached approximately 26,000, according to Ministry of Public Health sources. The fixed price of LL100,000 in the public sector caused the private sector to stick to the LL150,000 pricing, though the cost of administering the test is much lower.
- Most insurance companies do not cover testing (or hospital treatment) for the virus, as most standard contracts explicitly exclude epidemic coverage on the basis that it falls within the state’s responsibility.[8]
- As for the National Social Security Fund (NSSF), it issued a memorandum specifying that it would cover the test up to LL150,000 on the condition that the medical report of the person potentially infected include a high temperature, a severe cough, an acute headache, and severe shortness of breath.[9] In other words, all those potentially carrying the virus and not manifesting critical symptoms (as mentioned above, 80% of cases involve mild or no symptoms) are probably not covered.
Ensuring that testing is available on the broadest scale possible and free of charge is important because of its undoubtable effect in curbing the virus’ spread and reducing mortality. Access to testing is especially important during the phase of reduced home confinement, as widespread testing allows infected people to isolate. Countries that chose effective social distancing over home confinement and curfews, such as South Korea, ensured that testing was widely accessible.
Regarding coverage of medical treatment costs:
- In the initial stage, the NSSF covered infected people’s hospital expenses without covering the cost of personal protective equipment used by medical staff, causing some hospitals to refuse to recognize its coverage. Subsequently, the NSSF began covering these items, albeit only enough for four or five days of hospital treatment. Nevertheless, in most instances part of the costs – which in some private hospitals amounts to LL4 million for treatment in a regular room and LL 10 million for intensive care – still falls on the patients.
- Most insurance companies do not cover expenses for hospital treatment (or testing), as explained above. In this regard, the collective insurance contracts for engineers and doctors, for example, do not cover their hospital treatment expenses (or testing). Consequently, some professional syndicates, such as the Bar Association, decided to cover their members’ hospital treatment directly from the syndicate fund.
Regarding ensuring sick people’s access to treatment:
In the initial stage, private hospitals themselves opted not to treat the infected.[10] Hence, only people with certain privileges (such as political figures or the hospital’s own medical staff) received treatment in these hospitals. In an interview with Al Modon, President of the Syndicate of Private Hospitals Suleiman Haroun attributed this reluctance to the private hospitals’ fear that “other patients would be averse to entering the hospital”,[11] as well as the medical supplies crises that the country is witnessing amidst the financial and banking crisis.
However, as cases proliferated and the phobia that the virus initially caused declined, private hospitals realized the great profitability that the pandemic offers. Many created wings dedicated to treating COVID-19 patients, with costs reaching LL20 million for treatment in a regular room and LL30 million for intensive care.
With cases now steadily increasing (more than 3,000 new cases per day) and news about hospitals reaching their maximum capacity and the need to increase health sector readiness, a remarkable decision was issued on 5 January 2021 dictating a national lockdown from January 7 toFebruary 1. The decision, signed by General Secretary of the Council of Ministers Judge Mahmoud Makie, cited the decree extending the general mobilization to 31 March 2021 and the exigencies of public interest and safety, and mentioned that the president of the republic and the prime minister gave exceptional approval for it (though neither’s signature appeared). The decision includes many measures, among them “asking the ministers concerned to take the strictest measures that the law and general mobilization allow in order to compel private hospitals to establish intensive care beds earmarked for COVID-19 patients, including asking guarantors to cease working with hospitals that do not admit COVID-19 cases”. It also specified the number of intensive care beds that each private hospital must provide based on its classification, including twelve or more for university hospitals. While the decision raises many procedural questions, particularly concerning the power of the body that made it, it is the boldest step that the state has taken since the pandemic began to exercise the powers that the general mobilization decisions afford it. Yet the decision is still a timid move, as the punishment devised to address private hospitals’ refusal to comply with it (asking guarantors to cease working with them) is wholly inadequate.
The key question is, faced with the danger to public health and safety and the urgent need to raise health sector readiness when figures show that the occupancy rate has reached 86.4% for intensive care beds and 72.6% for beds earmarked for treating the infected,[12] will the state dare to take further steps? Will it seize uncooperative private hospitals or medical equipment, as allowed by the general mobilization[13] that the government declared on 15 March 2020 and as has occurred in other countries such as Spain?[14]
Given the situation described above, the state’s role in ensuring access to testing, medical treatment, and medicine (as well as means of complying with home confinement) free of charge for everyone, especially the most vulnerable groups (such as refugees and prisoners), appears pivotal. When viruses spread, they do not discriminate based on ethnicity, religion, social class, or nationality. This fact once again demonstrates the importance of reconsidering public policies and ensuring access to universal health coverage for all residents, as the health and social status of “others” directly affects every individual in society.
The Zuama and Political Parties Rush to Usurp the State’s Role: An Attempt to Reclaim Positions of Power
As the pandemic’s effects became evident, the zuama and traditional political parties began a counterattack to regain their grip over society and recover their usual position in the public arena after the October 17 uprising had managed to trigger its decline.
The fear generated by the pandemic, particularly due to the state’s weak capabilities and the reality embedded in Lebanese people’s shared memory that “the state is incapable” because of the public policies adopted, was a golden opportunity for the zuama and political parties to reclaim their positions and swoop in on the role of the “weak” state. Hence, they (alongside bank owners and some businessmen with vested interests, such as Wissam Achour) began a broad process of exploiting the current situation to buy loyalties and obtain more time to reestablish their grip over the social situation. In particular, they donated to public hospitals and paramedic services, put buildings or hotels at the disposal of the Ministry of Public Health, and mobilized their medical, health, and charity branches.[15]
For example, when acting Minister of Public Health Hamad Hasan was asked about securing the necessary beds to quarantine Lebanese expatriates in an interview on Al Jadeed TV (4 April 2020) on the eve of the return of the first batch, he said that 80% had been secured, deliberately mentioning that Parliament Speaker Nabih Berri and the Free Patriotic Movement had each provided a hotel. Similarly, Najib Mikati[16] donated[17] LL80 million to the Tripoli Governmental Hospital, Walid Jumblatt[18] donated USD500,000 to the Rafik Hariri University Hospital and USD100,000 to the Red Cross, and the Association of Banks in Lebanon donated USD6 million to purchase 120 ventilators and prepare COVID-19 wings in public hospitals in various governorates.
Finally, in a televised interview on 3 January 2021, Hasan mentioned, while commenting on a diagram of case distribution across districts, that most have been recorded in areas with Christian majorities and that he had therefore contacted Patriarch Bechara Boutros al-Rahi and intended to visit him.
Toward Reinforcing the Gains of October 17: Only the Social Welfare State Protects Society
The new crisis requires us to draw lessons, develop public policies that strengthen the social safety net, and consolidate the legitimacy of the state and its social function. This begins by safeguarding the right to health and ensuring universal access to public healthcare systems (alongside the other fundamental socioeconomic rights, such as education, work, and social protection). This challenge is not unique to Lebanon; rather, it has global dimensions. Talk of “the return of the welfare state”, which is being portrayed as the only entity capable of protecting society amidst crises like this one, is returning strongly to the fore. In this regard, a distinction has emerged between measures that states have adopted to combat the pandemic:[19] while neoliberal systems, governed by the interests of a select few, put all efforts into “flattening the curve” via various forms of confinement that place the entire burden and responsibility on individuals, the social welfare state works to “raise the readiness” of health systems. Austerity policies in public spending on the health sector have, it turns out, made many “developed” states vulnerable to the virus and led to record numbers of victims.[20]
In this regard, then-minister of labor Charbel Nahas proposed a bill in 2011 to provide universal health coverage for all residents irrespective of their legal employment status. He recommended funding this bill via taxes, particularly on banking and real estate revenue, after abolishing social security contributions.[21] Although the bill was aborted by the ruling system, its merit as the foundation of a social security net and the considerations upon which it was based are returning to the fore today. These considerations included the need “to create policies that reduce the burdens on factors of production and promote job creation and formality; hence, abolishing these contributions and funding universal health coverage via the public budget runs in this vein”.[22]
Of course, attempts today to achieve the goal of Nahas’ bill require adapting the sources of funding that were available then with the current bankruptcy of the state and creating new systems of public funding, such as an exceptional capital tax, which would rebuild a reservoir of state capacities. While there is no room to detail such systems here, other articles in The Legal Agenda have addressed this issue.
I shall conclude with a question: Will the current system, based on an alliance between the zuama and a select few monopolizing wealth, succeed in exploiting the current circumstances to reproduce itself and its domination over our lives through subordination, clientelism, and patronage? Or is this moment an opportunity to thwart this attempt and direct discussion toward the need to sow a citizen-state relationship based on rights, beginning with the right to health and to protect the gains of October 17, which requires developing the public services?
This article is an edited translation from Arabic.
[1] The right to health is a human right enshrined in international charters and laws, particularly Article 25 of the Universal Declaration of Human Rights (UDHR) and Article 12 of the International Covenant on Economic, Social and Cultural Rights (ICESCR).
[2] Another perspective deems that the Lebanese system has not changed since the establishment of Greater Lebanon (a sectarian quota-sharing system) while considering specific periods, particularly the 1958-1964 Fouad Chehab era, which witnessed the establishment of laws and institutions that shaped the welfare state, to be exceptions.
[3] See, in particular, Article 22 of the UDHR and Article 9 of the ICESCR.
[4] On this point, see Muhammad Hamdan’s unpublished study prepared as part of the “Haqqi ‘Alayya” campaign.
[5] Article 2 of Ministry of Public Health Regulation Decree no. 8377, issued on 30 December 1961.
[6] See the list of hospitals qualified to administer the test published by the Ministry of Public Health on 3 April 2020.
[7] On 4 April 2020, LAU Medical Center-Rizk Hospital announced a mobile clinic service to administer PCR tests in peripheral regions free of change for people without health coverage or insurance or unable to afford other testing. It began its operations from the Nabatieh Governmental Hospital.
[8] One of the reasons may be the disastrous financial effects on the companies given the number of clients who may have to be admitted to hospital.
[9] Media memorandum, 11 March 2020.
[10] Azza Hajj Hassan, “Idha Tafashsha Corona fi Lubnan: Hadhihi Hal Mustashfayatina”, Al Modon, 23 February 2020.
[11] Ibid.
[12] As of 5 January 2021.
[13] Legislative Decree no. 52/1983.
[14] Thomas Lemahieu, “L’Espagne n’hésite pas à réquisitionner”, L’Humanité, 17 March 2020.
[15] Tamirace Fakhoury, “Political Parties and Redistributive Power in the Lebanese State”, Lebanese Center for Policy Studies, April 2020.
[16] Former prime minister and current MP.
[17] This he did during a special episode organized by journalist Marcel Ghanem and MTV on 20 November 2020.
[18] Former minister and MP, and head of the Progressive Socialist Party.
[19] Gaël Giraud, “Covid-19: le retour de l’Etat-providence?”, Libération, 26 March 2020.
[20] “Ce qui les distingue, c’est leur rapport à la droite horizontale. Cette dernière ne tombe pas du ciel : elle est le résultat des politiques de santé publique menées au cours des décennies qui ont précédé. En France, nous disposons d’un lit de réanimation pour 13 600 personnes. En Italie, 1 pour 17 000. Outre-Rhin, 1 pour 8 300. Si aujourd’hui des Français meurent du coronavirus, c’est parce que trois décennies d’austérité budgétaire ont réduit la capacité de charge de notre système hospitalier public… L’Etat néolibéral, capturé par les intérêts privés de quelques-uns, considère la courbe horizontale comme une donnée «naturelle», intangible. Il n’a pas «d’argent magique» pour financer ses hôpitaux, accroître leur capacité d’accueil, sauver des vies. Il ne lui reste alors qu’à tenter d’agir sur la seule courbe grise en pratiquant, ou non, diverses variantes de confinement”, ibid.
[21] The presentation introducing the bill on 2 November 2011 stated that “universal health coverage funded via the public budget is one component of the social wage” and allows “the state’s legitimacy and role to be restored, social solidarity to be translated into practice, the use of resources to be corrected, and the purchasing power of families and the domestic business market to be expanded”.
[22] Rationale for the health coverage bill submitted by Minister of Labor Charbel Nahas, 2011.
Mapped through:
Articles, Inequalities, Discrimination and Marginalisation, Lebanon, Lebanon Magazine, Magazine, Private Sector, Public Institutions, Right to Health
Related Articles